Expert Video: Overview of the Underlying Pathophysiology of Migraine
Expert Video: Overview of the Underlying Pathophysiology of Migraine
What biological pathways underlie the symptoms associated with migraine?
World-renowned expert Andrew Charles, MD, discusses the biological pathways that underlie the symptoms associated with how migraine is more than just a headache in this short video

Overview of the Underlying Pathophysiology of Migraine
Clinical Phases of Migraine
Recent studies have shown that several anatomic regions and molecular pathways underlie the multifaceted symptoms across all phases of migraine.1-4

PRODROME
Activation of the hypothalamus, as well as neuropeptides involved in homeostatic functions, may contribute to symptoms experienced during the prodrome phase5
The hypothalamus is involved in a number of physiologic processes, including:6
- Nociceptive processing
- Control of the sleep–wake cycle
- Feeding
- Thirst
- Arousal
- Autonomic and endocrine regulation

Studies have shown the activation of the hypothalamus occurs prior to the onset of migraine pain.7,8
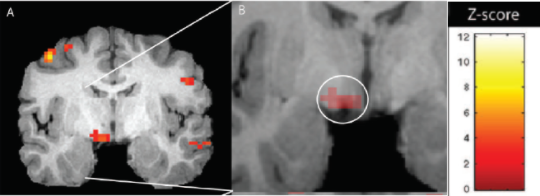
Brain activations in the early premonitory phase7
![]()
Reproduced from Maniyar et al.7 with permission from Oxford University Press.
Shown are areas of increased regional cerebral blood flow in the early premonitory phase greater than baseline in nitroglycerin-induced migraine. The results are superimposed on an anatomic reference derived from a representative T1-weighted MRI of one of the patients. Activation in the posterior hypothalamic region is highlighted by the circle. The color bar indicates the color coding of the Z-scores. Images are displayed in radiologic convention (ie, the left side of image shows the right side of the brain).7

It has been suggested that hypothalamic neurons that regulate homeostasis may underlie burdensome non-pain symptoms that occur during the prodrome phase and in other migraine phases, including:5-7,9
- Nausea and vomiting
- Changes in appetite
- Fatigue

AURA
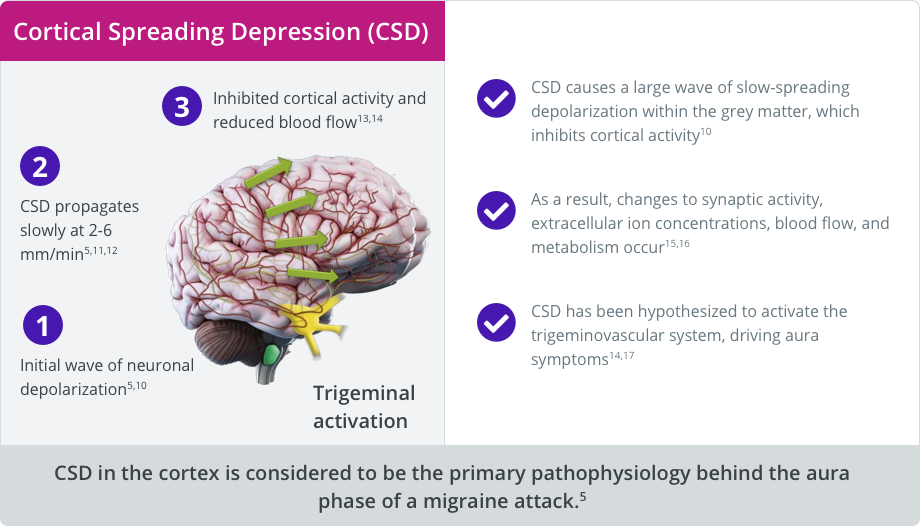
Cortical spreading depression (CSD) is considered to be the primary pathophysiology behind the aura phase.5,10
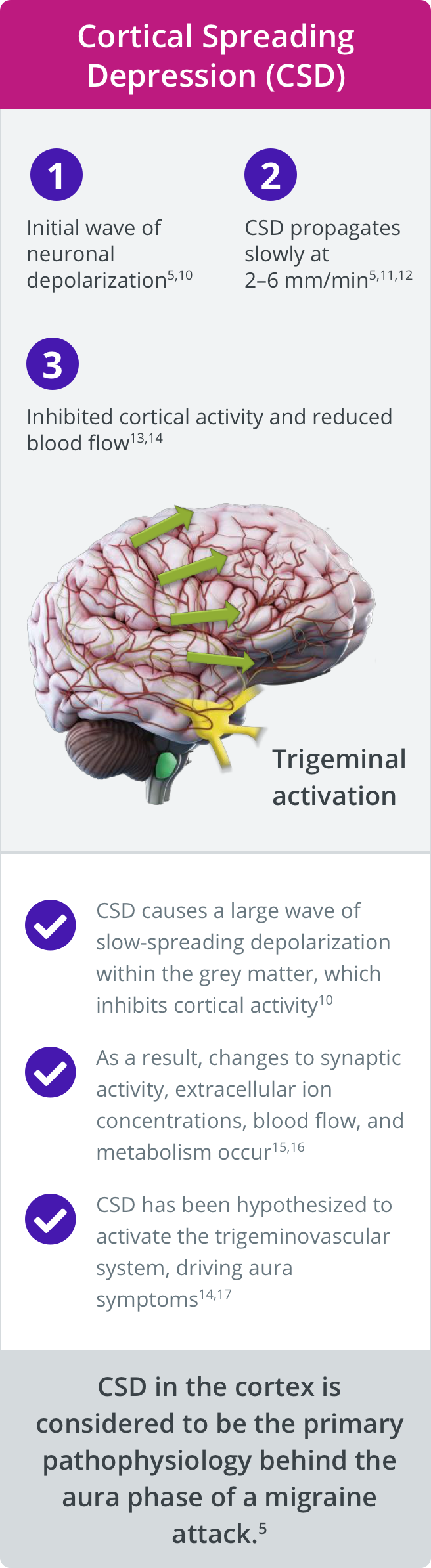

HEADACHE (ICTAL)
Several neuropeptides have been implicated in the sensitization of the central and peripheral trigeminovascular system, creating a state of hypersensitivity and contributing to both pain and non-pain symptoms during the headache phase.5
Several neuropeptides, including calcitonin gene-related peptide (CGRP), have been implicated in head pain and other symptoms.1
Preclinical expression studies suggest that CGRP and its receptor are expressed in multiple anatomic regions relevant to migraine (eg, trigeminovascular and cranial parasympathetic systems).1,18-20
Clinical evidence suggests that CGRP is involved in migraine pain.
- Plasma CGRP levels increase significantly during migraine attacks and return to normal following relief of migraine pain with triptan therapy1,21-24
- Infusion of CGRP can induce migraine-like attacks in patients with migraine25-27
- Approved therapeutics that target CGRP effectively reduce migraine attacks28-31
Neuropeptides may play a fundamental role in neurogenic inflammation, and peripheral and central sensitization of the trigeminovascular and other systems.1,18,32
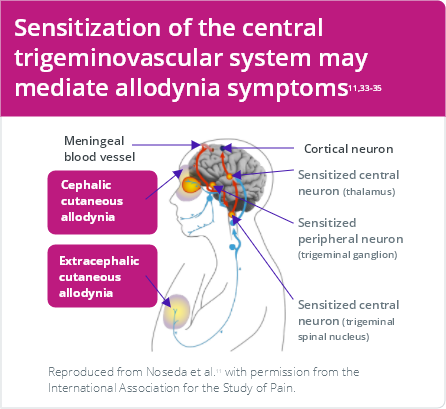
Functional and anatomic abnormalities are associated with sensitization and symptoms such as allodynia.33-35

Sensitization of primary nociceptors and central trigeminovascular neurons may contribute to allodynia in migraine33-35

Magnetic resonance imaging (MRI) studies have also demonstrated that patients with migraine and greater symptoms of allodynia may display structural abnormalities within the brainstem4

This suggests that altered sensory processing and brainstem structure may contribute to the severity of allodynia and hypersensitivity to the pain observed in migraine4

Sensitization of peripheral and central structures may be involved in photophobia.36
Proposed neural basis of photophobia in migraine5
Retinal and trigeminal nociceptive input converge in the thalamus…5,36,37


…which projects to the nociceptive areas of the cortex (S1/S2)5,36,37
…which can result in the exacerbation of migraine headache by light5,36,37
Hypersensitized visual cortex (V1/V2) may also contribute to this effect5,36,37

POSTDROME
There are a number of similarities in the symptoms experienced during the prodrome and postdrome phases.5,38 However, the precise pathophysiological events that underlie these symptoms remain uncertain.5,38
Prodrome symptoms, such as fatigue, food cravings, and cognitive symptoms may endure well into the aura, headache, and even postdrome phases of a migraine attack39-42
Overlap between prodromal and postdromal symptoms raises the possibility that symptoms may continue to occur throughout the attack but are overshadowed by the pain, nausea, and aura experienced during the headache phase5,43

Further research is required to understand the neurologic events that occur in the hours before and after a migraine headache5,43

INTERICTAL
Some regions of the brain remain abnormally activated after headache cessation, including the olfactory regions, the midbrain, and the hypothalamus.44-47
Functional imaging studies have demonstrated that multiple brain regions may remain active during the interictal period.44
STUDY: H2O15 PET was used to assess the cortical responses of 7 patients with migraine between attacks in response to heat pain and luminous stimulations.44
+ Light / - Pain
Activation of the visual cortex bilaterally was observed in patients with migraine but not in controls
Controls

No
pain
No
pain
Migraineurs

+ Light / + Pain
Concomitant pain stimulation potentiated visual cortex activation in patients with migraine
Controls

Pain
Pain
Migraineurs

Activations by light at 1800 Cd/m². Axial cross-sections at z=0, z=8, z=16 and z=24. Activations were in the cuneus, lingual gyrus, posterior cingulate cortex and precuneus. Note that the volume of activation is greater in migraineurs and that the activation in controls is more rostral.44
Role of the Trigeminovascular System in Migraine
The trigeminovascular system, which relays head pain signals to the brain, plays a key role in migraine pathophysiology and has components in the periphery (ie, outside the blood-brain barrier) as well as in the central nervous system (CNS) (ie, inside the blood-brain barrier).3,48-50
Migraine may occur as a result of a dysfunctional trigeminovascular system.11
Overview of the trigeminovascular system in migraine
Peripheral components5,51
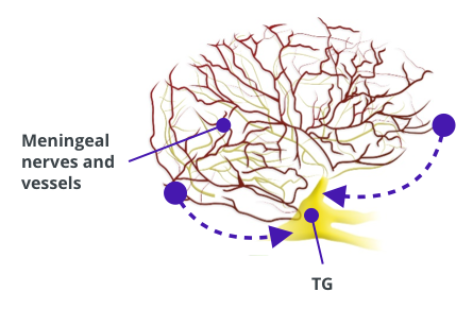
The trigeminal ganglion, located in the peripheral nervous system, relays trigeminovascular nociceptive input from the meningeal vessels and dura mater to the CNS5,51
Central components5
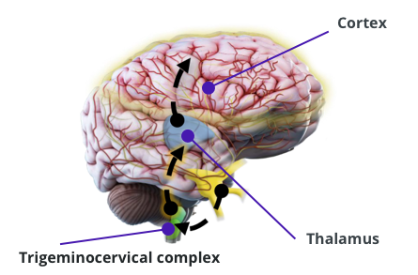
The trigeminocervical complex receives the peripheral trigeminovascular nociceptive pain signal from the trigeminal ganglion and relays it to the cortex via the thalamus, resulting in the experience of pain5,51
Activation of the other central regions, which project to/from the trigeminovascular system, can also contribute to non-pain symptoms5
Role of sensitization/hyperexcitability
- Pain is experienced when trigeminovascular neurons are activated and relay the migraine pain signal from the periphery to the CNS5
- Repeated activation of the trigeminovascular system over time results in a state of nervous system hypersensitivity and sustained pain5
-
Feedback from a sensitized brain may:5,52
- Potentiate pain signaling5,52
-
Contribute to common migraine symptoms5,52
- Photophobia, phonophobia, and cutaneous/mechanical allodynia
